The association between inflammation and bone loss and joint pain is now well recognised. Inflammation increases when oestrogen decreases.
Our sex hormones play a role in bone and cartilage metabolism. We have oestrogen receptors on bone cells and oestrogen interacts with cartilage growth factors. When levels of the antioxidant properties of oestrogen naturally fall during the menopause, joint protection can weaken, causing joint aches and stiffness. Unfortunately, it isn’t just arthralgia (joint stiffness) that menopausal women have to worry about.
Oestrogen fluctuations, as previously mentioned, increase joint inflammation. This can result in menopause-related osteoarthritis. And, those who go through early menopause are more likely to develop rheumatoid arthritis.
Adequate oestrogen levels are involved in maintaining immune-bone homeostasis: Bone loss and joint pain in menopause is very closely related to our immunity which is influenced by our intestinal microbiota or gut flora. Nearly 75% of our immune system activity is done through our gut and digestive tract. Your metabolism, hormonal levels, your mood, and cartilage/bone health can be affected by your gut flora.
What happens with drops in oestrogen?
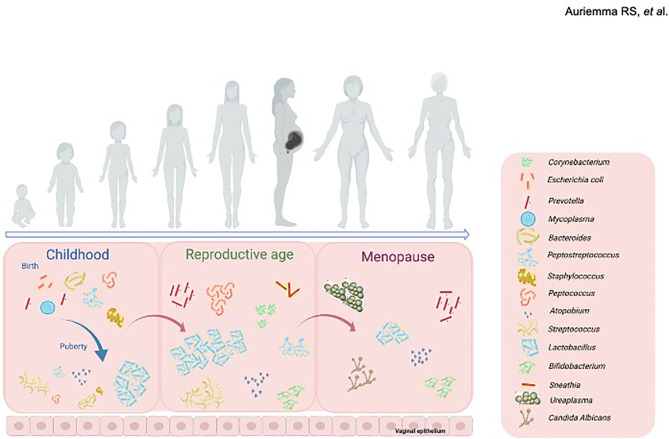
The absence of oestrogen alters the gut composition of positive bacteria and structure, leading to decreased diversity of species in your gut microbiome (see image). The falling oestrogen levels have therefore been associated with changes to the immune system and increased inflammatory markers = inflammation, joint pain and bone deterioration.
Oestrogen receptors present on the intestinal epithelium (gut cells) are involved in the maintenance of epithelial barrier (gut lining) integrity (think: leaky gut). They keep it healthy and prevent pathogens from creating inflammation.
Past studies have found that microbiota in the gut can affect how minerals such as calcium are absorbed. Other gut bacteria can regulate cell signaling and impact the bone remodeling process.
Probiotics are able to restore microbial diversity (although they are transient so only function whilst being taken), as well as giving positive support to gut integrity and immune response. Prebiotics help with calcium absorption.
Right now, there are a couple of theories on how the gut influences bone specifically.
Theory # 1 – Prebiotic Fibre: Many prebiotic fibres that can be found in everyday foods help maintain a healthy gut by feeding the friendly bacteria that are already there. Dietary fibre acts as a fertiliser for the probiotics that live in your gut (bifidobacteria in particular). Examples of prebiotic fibres we commonly eat are artichokes, dandelion greens, asparagus, and banana.
Theory # 2 – Immune System: We already know your gut protects your immune system. But, what does your immune system have to do with bones? Your immune system is responsible for regulating cytokines (inflammatory molecules), which play an important role in bone turnover (i.e., bone resorption and formation).
Although more research needs to be done, we do know changes in our gut microbiome affect aspects of our daily lives. A healthy gut can reduce inflammation and aid in nutrient absorption, including magnesium, vitamin D, and calcium, which are all great for your bones.
Having a healthy and balanced gut flora balance can help you digest foods and metabolise important nutrients that protect your overall well-being.
Altering your gut microbiota with increased good bacteria such as Lactobacillus and Bifidobacterium are thought to work in a few different ways to improve bone health.
- Increased mineral solubility through short-chain fatty acids.
- Production of phytase enzyme which binds and charges certain minerals such as phosphate, calcium, magnesium, iron, and zinc.
- Reduced inflammation throughout the gut and intestines.
All of these factors contribute to a better bioavailability of minerals for an overall healthy body and happy bones.
SUMMARY OF bone-healthy nutrients your gut microbiota is responsible for.
- Calcium: is paramount to healthy bones. Prebiotics have been shown to increase calcium-binding uptake protein. These calcium-binding proteins are critical for intracellular calcium functions, such as cell growth, cell differentiation, and transcription (making new parts!).
- Magnesium: possibly a lesser-known bone-health mineral, but it’s almost as important as calcium. Pairing magnesium with a calcium rich diet can preserve bone structure by drawing calcium out of the bloodstream and soft tissue and replacing it back into your bones.
- Vitamin D: Vitamin D also acts as an absorbing agent for calcium. Introducing vitamin D (which is actually a hormone and not a vitamin) into your system can get your gut microbiome to bone-healthy standards.
- Vitamin K: Produced by HEALTHY gut bacteria. Osteocalcin, the most important non-collagenous protein in bone, is vitamin K dependent and protects against brittleness
Whether you introduce good bacteria into your body through your diet or supplementation, it could be beneficial to your bone health. Alterations that enhance nutrients like vitamin D, K, magnesium and calcium are an attractive strategy to reduce the risk of bone diseases.
Specific PROBIOTICS:
L. plantarum HEAL9, L.plantarum HEAL19, and L. paracasei 8700:2: BIOME OSTEO PROBIOTIC showed 78% reduction in BONE LOSS in trial:
On the basis of encouraging preclinical results, a multicenter, randomised, double-blind, placebo-controlled trial was conducted to investigate the efficacy of these three probiotic strains on maintaining BMD in 249 healthy, early post-menopausal women. In women who were less than six years post-menopause, the effect of the probiotic was even more pronounced.
Useful links:
https://online.boneandjoint.org.uk/…/2046-3758.98.BJR…
https://oryon.co.uk/blog/osteoporosis-gut-health/