Hello all – The next couple of days, we look at bone health. This is such an important topic and should not be ignored. It can affect us all, and appears to be increasing in younger women.
I have uploaded a guide onto the membership page which is a great resource on bone health.
This is an area we need to be supporting from a young age, to have minimal deterioration later in life.
THE BASICS:
Bones are in a constant state of turnover, breaking down old bone cells and building new ones. However, bone breakdown tends to be faster than bone formation once we move into menopause and beyond.
Women lose 30 percent of the denser tissue that covers bones. Most of the loss occurs within the first decade after menopause, but both men and women lose 0.5 percent of bone density every year after age 50.
Osteoporosis is a disease characterised by low bone mass and micro deterioration of bone tissue = bone fragility and a consequent increase in fracture risk.
As there are no obvious symptoms of osteoporosis, the condition often goes undiagnosed until a minimal trauma fracture occurs. Fractures can lead to chronic pain, disability, loss of independence.
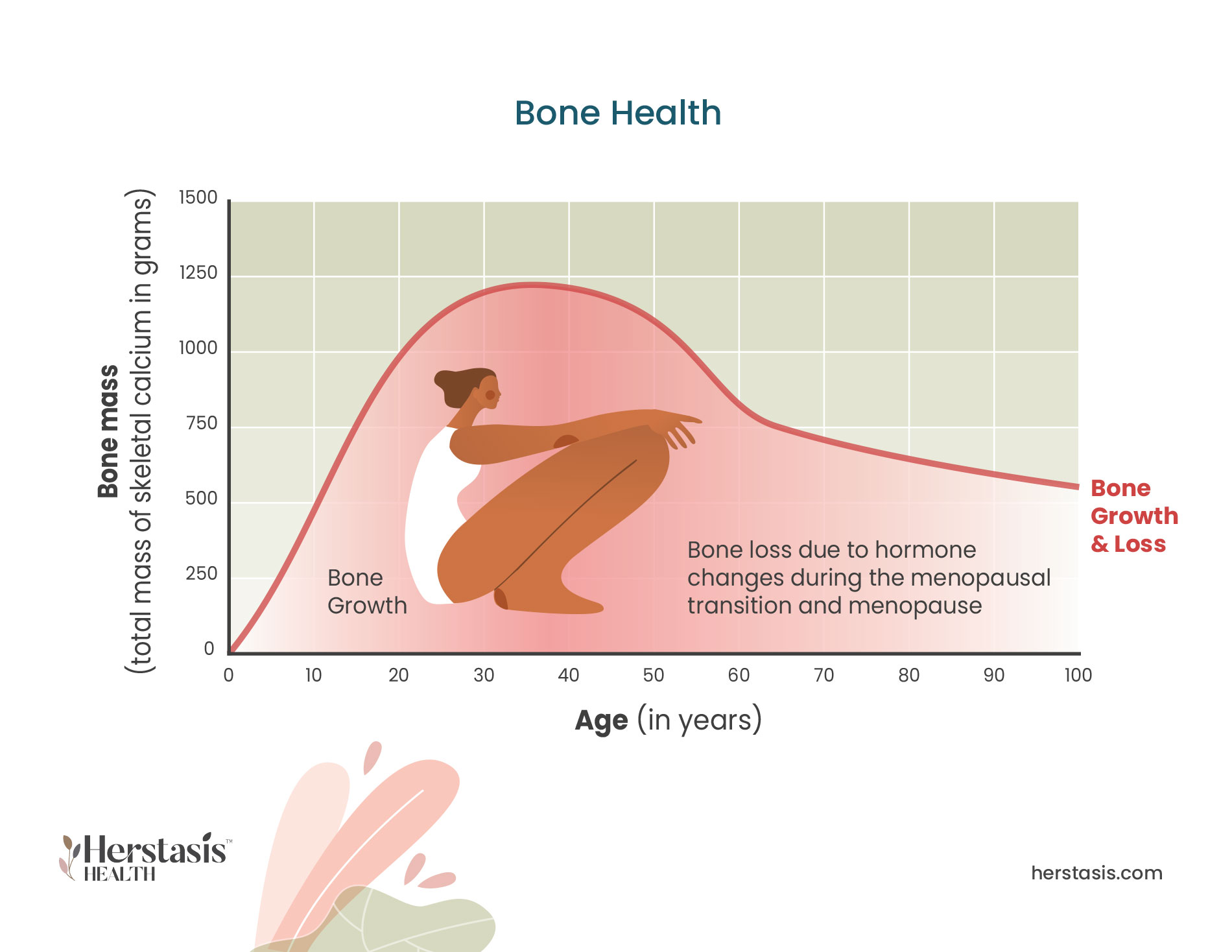
The risk of osteoporosis depends both on how much bone is acquired during skeletal growth and development until peak bone mass is reached at 20–30 years of age, and on the rate of the subsequent age-dependent bone loss.
The stronger your bones are in your twenties and thirties, the better off you’ll be when you reach the age at which bone density begins to decline.
The oral contraceptive pill (OCP) has an impact upon bone health later in life. Do listen to the recording with Tanya Borowski on this topic.
There is a 50% lifetime risk of osteoporotic fracture in women in the western world. It has long been known that declining oestrogen levels contribute to bone mineral loss. Sex Hormone Binding Globulin is a protein produced in the liver and binds oestrogen and testosterone. The steady rise of SHBG with ageing correlates with bone loss and osteoporosis. As a general rule the higher the SHBG level, the less oestrogen is available to contribute positively to bone health.
A woman’s risk of osteoporosis is determined largely by GENETIC factors (DNA from parents), age, and/or post-menopause factors. Genetics can account for 60-80% of our bone loss but can be modified by nutritional state and activity levels throughout childhood and early adulthood. The higher the peak mass acquired in youth, the lower the risk of osteoporotic fracture later in life.
Age-related loss naturally starts at a rate of 0.5-1% a year, after a person reaches their mid-thirties; in other words, after their bones have reached their peak bone mass and stabilised. For women, rapid bone loss of 1.5-3% a year occurs for five or six years around menopause before gradually slowing to 1% loss per year.
Risk factors associated with the development of osteoporosis include:
– Increasing age
– Menopause
– Family history of the condition
– Low vitamin D levels
– Dietary deficiency of calcium
– Low body weight
– Smoking
– Excess alcohol consumption
– Physical inactivity
– Long-term corticosteroid use
– Dysbiosis
– Chronic low-grade inflammation
How to prevent risk:
Exercise:
Weight-bearing exercises such as weight lifting (also called resistance training) and activities you do standing up — like walking, running, jogging, dancing, step aerobics, and tennis, are excellent ways to retain or build bone density. A minimum of 30 minutes of activity on most days of the week helps result in stronger, denser bones. Resistance training in particular helps build strong bones because the mechanical force of these exercises encourages the growth of new bone cells, according to a study published in Clinical Calcium in 2017.
You’ll get the most benefit if you vary the types of activities you do — which will make it more interesting, too.
Increase calcium intake… Calcium builds strong bones, and the best source is your diet. Good sources of calcium are fish such as sardines and salmon. Green leafy vegetables also have calcium, so eat kale, collard greens, Brussels sprouts, broccoli, Chinese cabbage and Tofu which has the highest amount of calcium per 100g.
Women ages 19 to 50 years old need about 1,000 milligrams of calcium a day. After menopause or age 50, increase that number to 1,200 milligrams of calcium a day.
Watch caffeine intake: Caffeine causes your body to excrete calcium more quickly. So drink less regular coffee, tea, and caffeinated soft drinks — and avoid high-caffeine energy drinks.
Drink only in moderation: Alcohol can lower your body’s ability to absorb calcium. If you do drink, strive for moderation
Get your vitamin D levels checked: Get your sunlight or take a supplement once levels are measured: Vitamin D enables the body to absorb calcium, and calcium is necessary for maintaining bone density. Magnesium is essential for absorption of Calcium and Vit D.
Avoid too much salt! Another reason to avoid packaged foods is that they often contain more salt: postmenopausal women who consume a lot of salt are at greater risk for osteoporosis, the bone-thinning disease, according to research published in the journal Osteoporosis International in January 2017.
MEDICATIONS known to DECREASE Bone Mineral Density:
Aromatase inhibitors (oestrogen cancer treatments), proton pump inhibitors, selective serotonin reuptake inhibitors (SSRI´s), anticonvulsants. Current or past use of glucocorticoid treatment for 3 months or longer
If you are not getting adequate Calcium/Vitamin D from diet and sunlight:
An analysis in 2013 showed that women taking HRT together with 1000mg Calcium per day and 400IU Vitamin D per day had greater bone protection than those taking HRT alone.
To support healthy levels of SHBG:
Increase protein intake may lower SHBG, Fish oil may help decrease levels, Good fibre consumption, Well functioning liver (avoid toxins etc), balance blood sugar.