Hitting off week 3 with a new term for you to remember – and often not discussed.
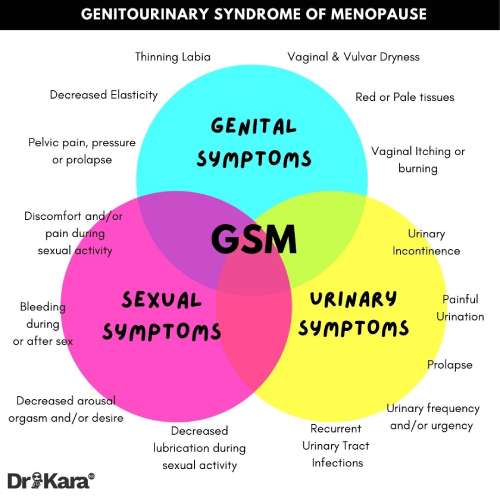
“Genitourinary syndrome of menopause” (GSM) is a medical and inclusive term that describes the multiple changes occurring in the vaginal size, pelvic floor tissues, bladder and urethra, and the loss of sexual function and libido, caused by lowered oestrogen levels during the menopause transition and post menopause.
These genitourinary changes primarily occur in response to reduced oestrogen levels. ‘Vaginal dryness’ sounds like a mild problem which might strike in your 60’s or 70’s (once the hot flushes have stopped), and causing a bit of bother in the bedroom. However, GSM is a condition that affects up to 70% of women at some time, peri- or postmenopause.
Symptoms of GSM include soreness, itching and burning pain in the vagina and/or vulva, and the need to wee, desperately or more frequently, that many women are led to believe is just a normal part of ageing they have to put up with. It can also mean more urinary tract infections (UTI), like cystitis. Signs and symptoms are illustrated below
Some facts not often spoken of:
- 50% of older women have pelvic organ prolapse (Gerten 2012)
- 1 out of 3 women suffer from sexual pain (Coady, 2015)
- 49% of all women leak urine (Markland, 2011)
Vaginal atrophy affects up to 47% of postmenopausal women, but symptoms are often underreported by patients due to embarrassment discussing “personal” symptoms or a belief that it is normal part of ageing (Hoffman et.al 2014). There are an estimated 2.4 million women in the UK living with vulval pain, according to the Vulval pain society.
TO AVOID STRESS ON THE VAGINA & MEMBRANES:
- Sterilise sex toys.
- Avoid perfumed pads, tampons with bleached cotton etc.
- Avoid perfumed shower gels on the vaginal area and avoid washing underwear in perfumed softeners.
- Avoid synthetic fibres in underwear.
- Finally manage your blood sugar levels which impacts the lactobacilli species.
Natural products that may offer relief with vaginal atrophy:
Lubrication is extremely important. You can consider a vaginal lubricant for intercourse, a moisteriser for daily use. INTO THE WYLDE is a natural range to consider.
https://intothewylde.com/
Weleda calendula nappy balm can be helpful as a barrier cream.
Oral collagen: vitamin C, zinc, vitamin A and vitamin E help maintain elasticity in the vagina.
Vitamin E Pessaries
- Vitamin E minimum 100iu: capsules vaginally daily over 12 weeks minimum
Vitamin E suppositories are suggested for relieving the symptoms of vaginal atrophy, especially in women who are unable to use hormone therapy or cope with the associated side effects (Parman et.al, 2016)
If the mucosal membrane is damaged, consider oral omega 7, 2 g per day orally.
Sea Buckthorn Oil – (see earlier post) 3gm oral dosage: 3 month trial duration
- Effects on pH of vagina (lowered)
- Improved Integrity of the vaginal epithelium
- Did not affect measures of burning, itch and irritation.
Black Cohosh/Actaea/Cimicifuga racemosa
- May improve vaginal dryness in postmenopausal women, as demonstrated in an improvement in the vaginal maturity index due to increased vaginal superficial cells (Wuttke et al. 2006)
Fennel/Foeniculum vulgare
- Fennel creams and or pessaries that contain hyaluronic acid may be helpful
A good resource: https://www.bashh.org/guidelines
https://pubmed.ncbi.nlm.nih.gov/36270905/
ZOE PREDICT STUDY FROM 2022
The role of diet on menopausal symptoms is discussed in this link. In a nut shell, eat plenty of different veggies of all colours and make sure to include healthy sources of fats from avocados, oily fish, nuts and eggs:
https://onlinelibrary.wiley.com/doi/epdf/10.1111/nbu.12607